- Home
- About Us
- Treatments
- Testimonials
- Media
- International Patient
- Blog
- Cases
- Contact
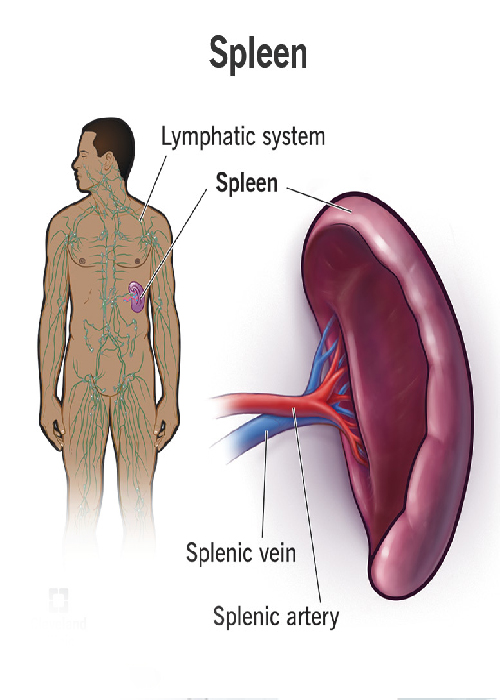
The spleen is a blood-filled organ located in the upper left abdominal cavity. It is a storage organ for red blood cells and contains many specialized white blood cells called macrophages (disease-fighting cells) which act to filter blood. The spleen is part of the immune system and also removes old and damaged blood particles from your system. The spleen helps the body identify and kill bacteria. The spleen can affect the platelet count, the red blood cell count, and even the white blood count. Piles Doctor in Ahmedabad
There are several reasons why a spleen might need to be removed, and the following list, though not all-inclusive, includes the most common reasons: The most common reason is a condition called idiopathic (unknown cause) thrombocytopenia (low platelets) purpura (ITP). Platelets are blood cells which aid in blood clotting. Hemolytic anemia (a condition that breaks down red blood cells) requires a spleen removal to prevent or decrease the need for transfusion. Also, hereditary (genetic) conditions that affect the shape of red blood cells, conditions are known as spherocytosis, sickle cell disease or thalassemia may require splenectomy. Often patients with cancers of the cells which fight infection, known as lymphoma or certain types of leukemia, require spleen removal. When the spleen gets enlarged, it sometimes removes too many platelets from your blood and has to be removed. Sometimes the blood supply to the spleen becomes blocked (infarct) or the artery abnormally expands (an aneurysm) and the spleen needs to be rem. Piles Doctor in Ahmedabad
How soon you are allowed to drink liquids and eat food after your
adhesiolysis operation depends on the extent of adhesiolysis. Generally, you will be allowed
to drink fluids within 6 – 8 hours after the operation. You may be given a saline drip for
that period. In the first 12 – 16 hours after recovery you may experience some nausea, but
this soon passes away.An evaluation typically includes a complete blood count (CBC), a
visual look at the blood cells placed on a glass slide called a smear, and often a bone
marrow examination.
Sometimes an ultrasound examination of spleen or a computerized
tomography (CT scan) is needed to know the underlying cause. LAPAROSCOPIC SPLEEN SURGERY A
cannula (hollow tube) is placed into the abdomen by your surgeon and your abdomen will be
inflated with carbon dioxide gas to create a space to operate. A laparoscope (a tiny
telescope connected to a video camera) is put through one of the cannulas which projects a
video picture of the internal organs and spleen on a television monitor. Several cannulas
are placed in different locations on your abdomen to allow your surgeon to place instruments
inside your belly to work and remove your spleen. A search for accessory (additional)
spleens and then removal of these extra spleens will be done since 15% of people have small,
extra spleens. After the spleen is cut from all that it is connected to, it is placed inside
a special bag. The bag with the spleen inside is pulled up into one of the small, but
largest incisions on your abdomen.
The spleen is broken up into small pieces (morcellated)
within the special bag and completely removed. Laparoscopic Spleen Surgery PREPARATION FOR
SURGERY Our expert team members shall help you to prepare you for surgery. Pre-operative
testing in most cases, you will need some tests before your surgery. The tests routinely
used include: Blood tests to measure your blood counts, your risk of bleeding or infection,
how well your liver and kidneys are working and blood grouping, in case you need the blood
transfusion. Chest x-ray and ECG (electrocardiogram) to check your lungs and your hearts
electrical system. Immunisation: Immunization with a vaccine to help prevent bacterial
infections after the spleen is removed should be given two weeks before surgery, if
possible. Blood product Arrangement Blood transfusion and/or blood products such as
platelets are arranged depending on your condition. Anaesthetic Assessment before Surgery:
Our expert team of Anaesthetist will ask you questions pertaining to your health and to
assess your fitness for surgery.
You are requested to tell them in detail about your current
and past medical ailments, allergic reactions you have had in the past and current medicines
that you are taking like blood thinning medicine. This medicine should be stopped prior to
surgery to minimize the risk of bleeding during /after surgery. Informed Consent Informed
consent is one of the most important parts of getting ready for surgery. It is a process
during which you are told about all aspects of the treatment before you give written
permission to perform the surgery. Getting ready for Surgery Depending on the type of
operation you have, there may be things you need to do to be ready for surgery: Emptying
your stomach and bowels (digestive tract) is important. Vomiting while under anesthesia can
be very dangerous because the vomitus could get into your lungs and cause an infection.
Because of this, you will be asked to not eat or drink anything starting the night before
the surgery or at least 6 hours before surgery. Laxative: You may also be asked to use a
laxative or an enema to make sure your bowels are empty. Shaving of the Operative part: You
need to have an area of your body shaved to keep hair from getting into the surgical cut
(incision). The area will be cleaned before the operation to reduce the risk of infection.
ANESTHESIA Anaesthesia is the use of drugs to make the body unable to feel pain for a period
of time. General anesthesia puts you into a deep sleep for the surgery. It is often started
by having you breathe into a face mask or by putting a drug into a vein in your arm. Once
you are asleep, an endotracheal or ET tube is put in your throat to make it easy for you to
breathe. Your heart rate, breathing rate, and blood pressure (vital signs) will be closely
watched during the surgery and Hernia Surgeon in Ahmedabad.
A doctor watches you throughout the procedure and until you wake
up. They also take out the ET tube when the operation is over. You will be taken to the
recovery room to be watched closely while the effects of the drugs wear off. This may take
hours. People waking up from general anesthesia often feel "out of it" for some time. Things
may seem hazy or dream-like for a while. Your throat may be sore for a while from the
endotracheal (ET) tube. RECOVERY FROM SURGERY Pain You may feel pain at the site of surgery.
We aim to keep you pain-free after surgery with the help of latest and most effective
technique or analgesic (pain relieving medicine). Eating and Drinking You will be allowed
orally liquids once you recover from the effect of anesthesia medicine and you don't have
nausea or vomiting. Gradually you can add soft to the normal diet. Activity Our healthcare
team will try to have you move around as soon as possible after surgery. You are encouraged
to get out of bed and walk the same day. While this may be hard at first, it helps speed
your recovery. It also helps your circulation and helps prevent blood clots from forming in
your legs. Going home Once you are eating and walking, and then you are ready to go home, in
most case in next day following surgery. Before leaving for home or health care team shall
give you detailed guidance regarding diet, activities, medications & further plan of
treatment RISKS & SIDE EFFECTS OF SURGERY There are risks that go with any type of medical
procedure and surgery is no longer an exception. The success of surgery depends upon 3
factors: type of disease/surgery, the experience of the surgeon and overall health of
patients. What's important is whether the expected benefits outweigh the possible risks.
Complications in major surgical procedures include: Complications related to Anaesthesia:
Reactions to drugs used (anesthesia) or other medicines. Although rare, these can be serious
because they can cause dangerously low blood pressures. Complications related to underlying
medical illness like heart disease, diabetes, kidney disease, obesity, malnutrition.
Complications related to Specific Operations: Possible complications may include cannula
site infections, pneumonia, internal bleeding or infection inside the abdomen at the site
where the spleen used to be, although these complications are infrequent. Laxative: You may
also be asked to use a laxative or an enema to Injury to the stomach, pancreas or internal
organs. You are encouraged with discussing in detail with our health care team before you
give your consent for surgery. Conversion to open surgery: In a small number of patients,
the laparoscopic method is not feasible because of the inability to visualize or handle the
organs (appendix) effectively.
Factors that may increase the possibility of converting to
the open procedure may include a perforated & densely adherent appendix to a nearby organ,
obesity, a history of prior abdominal surgery causing dense scar tissue, or bleeding
problems during the operation. The decision to convert to an open procedure is strictly
based on patient safety. The side effect of Surgery: Most people who have their spleens
removed have no clinical side effects. Only few may have the following condition. They are
advised to inform about spleen surgery to their family doctor when they consult for any
medical ailments. Overwhelming Post-Splenectomy Infection (OPSI): There are certain
bacterial infections that people are more susceptible to after a splenectomy. This is
particularly important in younger patients, and it is important to seek medical attention
early if an infection develops. The incidence of these bacterial infections overall is
uncommon. Preoperative vaccinations against the bacteria are normally administered to help
decrease this incidence - Piles Doctor in Ahmedabad.
It may be given after surgery if emergency surgery was done.
Antibiotics, like penicillin, is given after surgery for some time to prevent infection.
Don't neglect if have a fever after surgery. Report to your to the family doctor and tell
him that your spleen has been removed. So he gives you proper treatment. Thrombocytosis: The
platelet count can also rise after splenectomy and should be monitored. Patients
occasionally have to take aspirin products to help reduce the function of platelets. LIFE
AFTER SURGERY Nutrition Our healthcare team shall advise you in detail regarding dietary
habits, Briefly, your diet begins with liquids followed by the gradual advance to solid
foods. Exercise Patients are encouraged to engage in light activity while at home. You will
be able to get back to your normal activities within a short amount of time (week). Follow
up You may be advised to see our healthcare team after 1 week to assess your progress and to
address your problems.

User visits the website and navigates to the "Appointment Booking" section.
After completing the form, the user submits their appointment request.
If the requested slot is available, the administrative staff confirms appointment.