- Home
- About Us
- Treatments
- Testimonials
- Media
- International Patient
- Blog
- Cases
- Contact
App The colon and rectum are parts of the digestive system. They form a long, muscular tube called the large intestine (also called the large bowel). The colon is the first 4 to 5 feet of the large intestine, and the rectum is the last several inches. Partly digested food enters the colon from the small intestine. The colon removes water and nutrients from the food and turns the rest into waste (stool). The waste passes from the colon into the rectum and then out of the body through the anus. Tumors can be benign or malignant: Piles Doctor in Ahmedabad
Cancer cells spread by entering the bloodstream or the lymphatic system. The cancer cells form new tumors that damage other organs. The spread of cancer is called metastasis. When colorectal cancer spreads outside the colon or rectum, cancer cells are often found in nearby lymph nodes. If cancer cells have reached these nodes, they may also have spread to other lymph nodes or other organs. Colorectal cancer cells most often spread to the liver. When cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the original tumor. For example, if colorectal cancer spreads to the liver, the cancer cells in the liver are actually colorectal cancer cells. The disease is metastatic colorectal cancer, not liver cancer. For that reason, it is treated as colorectal cancer, not liver cancer. Doctors call the new tumor "distant" or metastatic disease. Piles Doctor in Ahmedabad
Studies have found the following risk factors for colorectal cancer: 1. Age over 50: Colorectal cancer is more likely to occur as people get older. More than 90 percent of people with this disease are diagnosed after age 50. The average age at diagnosis is 72. 2. Colorectal polyps: Polyps are growths on the inner wall of the colon or rectum. They are common in people over age 50. Most polyps are benign (not cancer), but some polyps (adenomas) can become cancer. Finding and removing polyps may reduce the risk of colorectal cancer. 3. The family history of colorectal cancer: Close relatives (parents, brothers, sisters, or children) of a person with a history of colorectal cancer are somewhat more likely to develop this disease themselves, especially if the relative had cancer at a young age. If many close relatives have a history of colorectal cancer, the risk is even greater. 4. Genetic alterations: Changes in certain genes increase the risk of colorectal cancer. 5. Hereditary nonpolyposis colon cancer (HNPCC) is the most common type of inherited (genetic) colorectal cancer. It accounts for about 2 percent of all colorectal cancer cases. It is caused by changes in an HNPCC gene. Most people with an altered HNPCC gene develop colon cancer, and the average age at diagnosis of colon cancer is 44. 6. Familial adenomatous polyposis (FAP) is a rare, inherited condition in which hundreds of polyps form in the colon and rectum. It is caused by a change in a specific gene called APC. Unless FAP is treated, it usually leads to colorectal cancer by age 40. FAP accounts for less than 1 percent of all colorectal cancer cases. Family members of people who have HNPCC or FAP can have genetic testing to check for specific genetic changes. For those who have changes in their genes, health care providers may suggest ways to try to reduce the risk of colorectal cancer or to improve the detection of this disease. For adults with FAP, the doctor may recommend an operation to remove all or part of the colon and rectum. 1. Personal history of cancer: A person who has already had colorectal cancer may develop colorectal cancer a second time. Also, women with a history of cancer of the ovary, uterus (endometrium), or breast are at a somewhat higher risk of developing colorectal cancer. 2. Ulcerative colitis or Crohn disease: A person who has had a condition that causes inflammation of the colon (such as ulcerative colitis or Crohn's disease) for many years is at increased risk of developing colorectal cancer. 3. Diet: Studies suggest that diets high in fat (especially animal fat) and low in calcium, folate, and fiber may increase the risk of colorectal cancer. Also, some studies suggest that people who eat a diet very low in fruits and vegetables may have a higher risk of colorectal cancer. However, results from diet studies do not always agree, and more research is needed to better understand how diet affects the risk of colorectal cancer. 4. Cigarette smoking: A person who smokes cigarettes may be at increased risk of developing polyps and colorectal cancer. Because people who have colorectal cancer may develop colorectal cancer a second time, it is important to have checkups. If you have colorectal cancer, you also may be concerned that your family members may develop the disease. People who think they may be at risk should talk to their doctor. The doctor may be able to suggest ways to reduce the risk and can plan an appropriate schedule for checkups. See the "Screening" section to learn more about tests that can find polyps or colorectal cancer. Piles Doctor in Ahmedabad
A common symptom of colorectal cancer is a change in bowel habits. Symptoms include: 1. Having diarrhea or constipation. 2. Feeling that your bowel does not empty completely. 3. Finding blood (either bright red or very dark) in your stool. 4. Finding your stools are narrower than usual. 5. Frequently having gas pains or cramps, or feeling full or bloated. 6. Losing weight for no known reason. 7. Feeling very tired all the time. 8. Having nausea or vomiting. Most often, these symptoms are not due to cancer. Other health problems can cause the same symptoms. Anyone with these symptoms should see a doctor to be diagnosed and treated as early as possible. Usually, early cancer does not cause pain. It is important not to wait to feel pain before seeing a doctor. Hernia Surgeon in Ahmedabad
If you have screening test results that suggest cancer or you have symptoms, your doctor must find out whether they are due to cancer or some other cause. Your doctor asks about your personal and family medical history and gives you a physical exam. You may have one or more of the tests described in the "Screening" section. If your physical exam and test results do not suggest cancer, your doctor may decide that no further tests are needed and no treatment is necessary. However, your doctor may recommend a schedule for checkups. If tests show an abnormal area (such as a polyp), a biopsy to check for cancer cells may be necessary. Often, the abnormal tissue can be removed during colonoscopy or sigmoidoscopy. A pathologist checks the tissue for cancer cells using a microscope.
If the biopsy shows that cancer is present, your doctor needs to know the extent (stage) of the disease to plan the best treatment. The stage is based on whether the tumor has invaded nearby tissues, whether cancer has spread and, if so, to what parts of the body. Your doctor may order some of the following tests: 1. Blood tests: Your doctor checks for carcinoembryonic antigen (CEA) and other substances in the blood. Some people who have colorectal cancer or other conditions have a high CEA level. 2. Colonoscopy: If colonoscopy was not performed for diagnosis, your doctor checks for abnormal areas along the entire length of the colon and rectum with a colonoscopy. 3. Endorectal ultrasound: An ultrasound probe is inserted into your rectum. The probe sends out sound waves that people cannot hear. The waves bounce off your rectum and nearby tissues, and a computer uses the echoes to create a picture. The picture may show how deep a rectal tumor has grown or whether cancer has spread to lymph nodes or other nearby tissues. 4. Chest x-ray: X-rays of your chest may show whether cancer has spread to your lungs. 5. CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of areas inside your body. You may receive an injection of dye. A CT scan may show whether cancer has spread to the liver, lungs, or other organs. Your doctor may also use other tests (such as MRI) to see whether cancer has spread. Sometimes staging is not complete until after surgery to remove the tumor. (Surgery for colorectal cancer is described in the "Treatment" section.) Doctors describe colorectal cancer by the following stages: 1. Stage 0: The cancer is found only in the innermost lining of the colon or rectum. Carcinoma in situ is another name for Stage 0 colorectal cancer. 2. Stage I: The tumor has grown into the inner wall of the colon or rectum. The tumor has not grown through the wall. 3. Stage II: The tumor extends more deeply into or through the wall of the colon or rectum. It may have invaded nearby tissue, but cancer cells have not spread to the lymph nodes. 4. Stage III: cancer has spread to nearby lymph nodes, but not to other parts of the body. 5. Recurrence: This is cancer that has been treated and has returned after a period of time when cancer could not be detected. The disease may return in the colon or rectum, or in another part of the body.
The choice of treatment depends mainly on the location of the tumor in the colon or rectum and the stage of the disease.Treatment for colorectal cancer may involve surgery, chemotherapy, biological therapy or radiation therapy. Some people have a combination of treatments. These treatments are described below. Colon cancer sometimes is treated differently from rectal cancer. Treatments for colon and rectal cancer are described separately below. Your doctor can describe your treatment choices and the expected results. You and your doctor can work together to develop a treatment plan that meets your needs. Cancer treatment is either local therapy or systemic therapy: 1. Local therapy: Surgery and radiation therapy are local therapies. They remove or destroy cancer in or near the colon or rectum. When colorectal cancer has spread to other parts of the body, local therapy may be used to control the disease in those specific areas. 2. Systemic therapy: Chemotherapy and biological therapy are systemic therapies. The drugs enter the bloodstream and destroy or control cancer throughout the body. Because cancer treatments often damage healthy cells and tissues, side effects are common. Side effects depend mainly on the type and extent of the treatment. Side effects may not be the same for each person, and they may change from one treatment session to the next. Before treatment starts, your health care team will explain possible side effects and suggest ways to help you manage them.
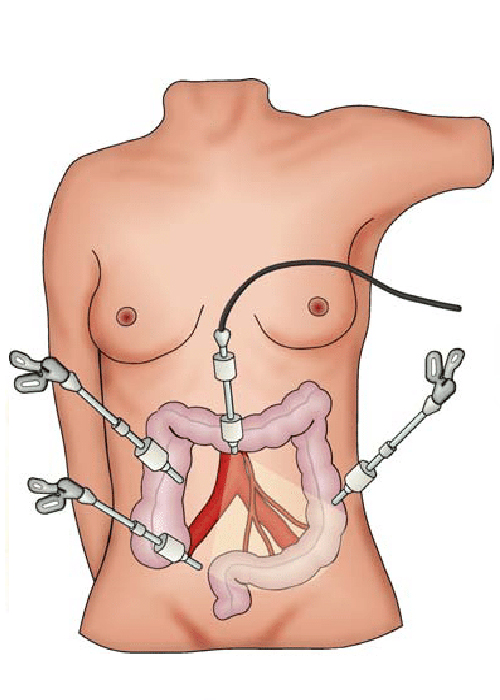
Surgery is the most common treatment for colorectal cancer. 1. Colonoscopy: A small malignant polyp may be removed from your colon or upper rectum with a colonoscopy. Some small tumors in the lower rectum can be removed through your anus without a colonoscopy. 2. Laparoscopy: Early colon cancer may be removed with the aid of a thin, lighted tube (laparoscope). Three or four tiny cuts are made into your abdomen. The surgeon sees inside your abdomen with the laparoscope. The tumor and part of the healthy colon are removed. Nearby lymph nodes also may be removed. The surgeon checks the rest of your intestine and your liver to see if cancer has spread. 3. Open surgery: The surgeon makes a large cut into your abdomen to remove the tumor and part of the healthy colon or rectum. Some nearby lymph nodes are also removed. The surgeon checks the rest of your intestine and your liver to see if cancer has spread. When a section of your colon or rectum is removed, the surgeon can usually reconnect the healthy parts. However, sometimes reconnection is not possible. In this case, the surgeon creates a new path for waste to leave your body. The surgeon makes an opening (stoma) in the wall of the abdomen, connects the upper end of the intestine to the stoma, and closes the other end. The operation to create the stoma is called a colostomy. A flat bag fits over the stoma to collect waste, and a special adhesive holds it in place. For most people, the stoma is temporary. It is needed only until the colon or rectum heals from surgery. After healing takes place, the surgeon reconnects the parts of the intestine and closes the stoma. Some people, especially those with a tumor in the lower rectum, need a permanent stoma. People who have a colostomy may have irritation of the skin around the stoma. Your doctor, your nurse, or an enterostomal therapist can teach you how to clean the area and prevent irritation and infection. The "Rehabilitation" section has more information about how people learn to care for a stoma. The time it takes to heal after surgery is different for each person. You may be uncomfortable for the first few days. Medicine can help control your pain. Before surgery, you should discuss the plan for pain relief with your doctor or nurse. After surgery, your doctor can adjust the plan if you need more pain relief. It is common to feel tired or weak for a while. Also, surgery sometimes causes constipation or diarrhea. Your healthcare team monitors you for signs of bleeding, infection, or other problems requiring immediate treatment. Chemotherapy.
Goal of Cancer Surgery Depending on your cancer type and stage, our goals for treatment are: 1. Cure: This is the most important goal of cancer surgery. In fact, as a cancer patient, you are also strongly willing to have the cure for cancer for forever. For most of the Liver & Gastro-intestinal cancers perhaps surgery is the first step for sure. Radiation &/or Chemotherapy may be advised as an additional tool to achieve this goal. 2. Control: If your cancer is at a later stage or if previous treatments have been unsuccessful, we aim to control your cancer by removing as much as safely possible. Once you recover from surgery, radiation or chemotherapy is advised as an important tool to control your cancer. 3. Comfort: If you have an advanced stage of cancer or one that hasn't responded to treatments and having symptoms because of tumor i.e pain, jaundice, vomiting, bleeding either in vomitus or in the stool, then our multi-specialist team work together to sure you are free of pain and other symptoms. Role of Surgery for Cancer treatment Surgery can be done for many reasons for treatment of cancer. Curative Surgery 1. Curative surgery is done when cancer is found in only one area, and it’s likely that all of the cancer can be removed. In this case, curative surgery can be the main treatment. It may be used alone or along with chemotherapy or radiation therapy, which can be given before or after the operation. Diagnostic & Staging Surgery 1. This type of surgery is used to take out a piece of tissue (biopsy) to find out if cancer is present or what type of cancer it is. The diagnosis of cancer is made by looking at the cells under a microscope. Staging surgery is done to find out how much cancer there is and how far it has spread. The physical exam and the results of lab and imaging tests are used to figure out the clinical stage of cancer. But the surgical stage (also called the pathologic stage) is usually a more exact measure of how far cancer has spread. Examples of surgical procedures commonly used to stage cancers, like laparoscopy or laparotomy. Palliative Surgery 1. This type of surgery is used to treat problems caused by advanced cancer. It is not done to cure cancer. For example, cancers of intestine may grow large enough to block off (obstruct) the intestine or tumor is bleeding and unable to control bleed by medical/endoscopic technique. If this happens, surgery can be used to remove the blockage/control bleeding. Approach to Surgery: How is surgery performed? (Special surgery techniques): Open Or Laparoscopic Open Surgery: 1. It is the Gold Standard approach for Liver & Gastro-Intestinal cancer. An incision is given on the belly depending Upton the underlying location of a tumor so that surgeon can directly approach cancer by cutting the belly. Open Surgery helps to remove tumor safely if its adherent to nearby blood vessels or organ, that is otherwise difficult in laparoscopic surgery. Laparoscopic Surgery 1. A laparoscope is a long, thin, flexible tube that can be put through a small cut (incision) to look inside the body. In recent years, doctors have found that by creating small holes and using special instruments, the laparoscope can be used to perform surgery without making a large cut. This can help reduce blood loss during surgery and pain afterward. It can also shorten hospital stays and allow people to heal faster. 2. The role of laparoscopic surgery in cancer treatment is not yet clear. Doctors are now studying whether it is safe and effective to use laparoscopic surgeries for cancers of the stomach, colon, rectum & liver. It may prove to be as safe and work as well as standard surgery while cutting less and causing less damage to healthy tissues (being less invasive). Biopsy of Cancer before Surgery A biopsy is a procedure to confirm the presence of cancer. It’s not essential before surgery. Usually a biopsy is performed when 1. Suspicion is cause other than cancer, 2. When surgery cannot be done for cancer due to the advanced stage of cancer or 3. The patient is unfit to undergo surgery. In this situation, biopsy guides for further therapy. If all investigations suggest that cancer can be removed in totality from a body, then the biopsy can be avoided in to minimize the risk of spillage of cancer cell during a biopsy procedure. There is the variety of way to perform biopsies: Fine Needle Aspiration (FAN) biopsy 1. Fine needle aspiration (FNA) uses a very thin needle attached to a syringe to pull out small bits of tissue. The needle is guided into the tumor by looking at it using an imaging test, like an ultrasound or CT scan. 2. The main advantage of FNA is that there is no need to cut through the skin, so there is no surgical incision. 3. A drawback is that in some cases the needle can’t take out enough tissue for an exact diagnosis. A more invasive type of biopsy (one that involves larger needles or a cut in the skin) may then be needed. Core Needle biopsy 1. This type of biopsy uses a larger needle to take out a core of tissue and done under the guidance of imaging tests like an ultrasound or CT scan. The advantage of core biopsy is that it usually collects enough tissue to find out whether the tumor is cancer. Excisional or Incisional biopsy 1. For these biopsies, the surgeon removes the entire tumor (excisional biopsy) or a small part of the tumor (incisional biopsy).
Our expert team members shall help you to prepare you for surgery. You are strongly advised to stop smoking, stop drinking alcohol, try to improve your diet, lose weight, or actively exercise before surgery. Pre-operative testing In most cases, you will need some tests before your surgery. The tests routinely used include: 1. Blood tests to measure your blood counts, your risk of bleeding or infection, and how well your liver and kidneys are working. Your blood group type is also be checked in case you need blood transfusions during the operation. 2. Chest x-ray and ECG (electrocardiogram) to check your lungs and your heart’s electrical system. 3. USG/CT scans/ MRI to look at the size and location of the tumors and see if cancer looks like it has spread to nearby tissues. Anaesthetic Assessment before Surgery: Our expert team of Anaesthetist will ask you questions pertaining to your health and to assess your fitness for surgery. You are requested to tell them in detail about your current and past medical ailments, allergic reactions you’ve had in the past and current medicines that you are taking like blood thinning medicine. This medicine should be stopped 1 week prior to surgery. Informed Consent Informed consent is one of the most important parts of “getting ready for surgery”. It is a process during which you are told about all aspects of the treatment before you give your doctor written permission to do the surgery. Getting ready for Surgery Depending on the type of operation you have, there may be things you need to do to be ready for surgery: 1. Emptying your stomach and bowels (digestive tract) is important. Vomiting while under anesthesia can be very dangerous because the vomit could get into your lungs and cause an infection. Because of this, you will be asked to not eat or drink anything starting the night before the surgery. 2. Laxative: You may also be asked to use a laxative or an enema to make sure your bowels are empty. 3. Shaving of the Operative part: You need to have an area of your body shaved to keep hair from getting into the surgical cut (incision). The area will be cleaned before the operation to reduce the risk of infection.
Our expert team members shall help you to prepare you for surgery. You are strongly advised to stop smoking, stop drinking alcohol, try to improve your diet, lose weight, or actively exercise before surgery. Pre-operative testing In most cases, you will need some tests before your surgery. The tests routinely used include: 1. Blood tests to measure your blood counts, your risk of bleeding or infection, and how well your liver and kidneys are working. Your blood group type is also be checked in case you need blood transfusions during the operation. 2. Chest x-ray and ECG (electrocardiogram) to check your lungs and your heart’s electrical system. 3. USG/CT scans/ MRI to look at the size and location of the tumors and see if cancer looks like it has spread to nearby tissues. Anaesthetic Assessment before Surgery: Our expert team of Anaesthetist will ask you questions pertaining to your health and to assess your fitness for surgery. You are requested to tell them in detail about your current and past medical ailmentAnaesthesia is the use of drugs to make the body unable to feel pain for a period of time. General anesthesia puts you into a deep sleep for the surgery. It is often started by having you breathe into a face mask or by putting a drug into a vein in your arm. Once you are asleep, an endotracheal or ET tube is put in your throat to make it easy for you to breathe. Your heart rate, breathing rate, and blood pressure (vital signs) will be closely watched during the surgery. A doctor watches you throughout the procedure and until you wake up. They also take out the ET tube when the operation is over. You will be taken to the recovery room to be watched closely while the effects of the drugs wear off. This may take hours. People waking up from general anesthesia often feel "out of it" for some time. Things may seem hazy or dream-like for a while. Your throat may be sore for a while from the endotracheal (ET) tube. RECOVERY FROM SURGERY Your recovery right after surgery depends on many factors, including your state of health before the operation and how extensive the operation was performed. Pain You may feel pain at the site of surgery. We aim to keep you pain-free after surgery with the help of latest and most effective technique or analgesic (pain relieving medicine). Tube/ Drains 1. You may also have Ryle’s Tube (tube going through the nose to stomach) that drain out intestinal fluid. This tube helps to relieve nausea and vomiting after surgery and usually removed 1-2 day after surgery. 2. You may also have “Tube” (called a Foley catheter) draining urine from your bladder into a bag. This will be taken out soon after surgery, once you are comfortable enough to go to the bathroom. 3. You may have a tube or tubes (called Drains) coming out of the surgical opening in your skin (incision site). Drains allow the excess fluid that collects at the surgery site to leave the body. Drain tube will also be removed once they stop collecting fluid, usually a few days after the operation. Leg Stocking / Compression boot As you remain in bed on the day of surgery, circulation of blood in leg become sluggish that may increase the possibility of thromboembolism. To minimise it, you will be wearing leg stocking/ pneumatic compression boot to improve your leg circulation thus minimising the risk of thrombosis. Eating and Drinking You may not feel much like eating or drinking, but this is an important part of the recovery process. Our healthcare team may start you out with ice chips or clear liquids. The stomach and intestines (digestive tract) are one of the last parts of the body to recover from the drugs used during surgery. You will need to have signs of stomach and bowel activity before you will be allowed to eat. You will likely be on a clear liquid diet until this happens. Once it does, you may get to try solid foods. Activity 1. Our healthcare team will try to have you move around as soon as possible after surgery. They may even have you out of bed and walking the same day. While this may be hard at first, it helps speed your recovery by getting your digestive tract moving. It also helps your circulation and helps prevent blood clots from forming in your legs. 2. Our team shall also encourage you to do deep breathing exercises. This helps fully inflate your lungs and reduces the risk of pneumonia. You are advised to take deep breaths and cough every hour to help prevent lung infections. You will use an incentive spirometer (a small device used in breathing exercises to prevent complications after major surgery) 10-15 times every hour. Going home Once you are eating and walking, all tube/drains placed during surgery are removed, and then you may be ready to go home. Before leaving for home or health care team shall give you detailed guidance regarding diet, activities, medications & further plan of treatment. RISKS & SIDE EFFECTS OF SURGERY There are risks that go with any type of medical procedure and surgery is no longer an exception. The success of surgery depends upon 3 factors: type of disease/surgery, the experience of the surgeon and overall health of patients. What’s important is whether the expected benefits outweigh the possible risks. Doctors have been performing surgeries for a very long time. Advances in surgical techniques and our understanding of how to prevent infections have made modern surgery safer and less likely to damage healthy tissues than it has ever been. Still, there’s always a degree of risk involved, no matter how small. Different procedures have different kinds of risks and side effects. Be sure to discuss the details of your case with our health care team, who can give you a better idea about what your actual risks are. During surgery, possible complications during surgery may be caused by the surgery itself, the drugs used (anesthesia), or an underlying disease. Generally speaking, the more complex the surgery is the greater the risk. Complications in major surgical procedures include: 1. Complications related to Anaesthesia : Reactions to drugs used (anesthesia) or other medicines. Although rare, these can be serious because they can cause dangerously low blood pressures. Your doctors will watch your heart rate, breathing rate, blood pressure, and other signs throughout the procedure to look for this. 2. Complications related to underlying medical illness like heart disease, diabetes, kidney disease, obesity, malnutrition. 1. Lung : Pneumonia, Atelectasis (collapse of lung), effusion (fluid in chest) can occur, especially in patients with reduced lung function, such as smokers. Doing deep breathing exercises as soon as possible after surgery helps lessen this risk. 2. Thrombosis (blood clot) in leg & embolism (blood clot) in lung :Blood clots can form in the deep veins of the legs after surgery, especially if a person stays in bed for a long time. Such a clot can become a serious problem if it breaks loose and travels to another part of the body, such as a lung. This is a big reason why you will be encouraged to get out of bed to sit, stand, and walk as soon as possible. 3. Cardiovascular: Myocardial infarction (heart attack), Arrhythmia (irregular heartbeat), Stroke (cerebrovascular accidents). 4. Kidney & urinary tract infection, acute kidney failure if patient has uncontrolled/non-responding infection. 3. Complications related to Specific Operations 1. There are specific complications related to type of surgery. You are encouraged with discuss in detail with our health care team before you give your consent for surgery. 2. Bile leak 3. Bleed 4. Complications related to Major Surgery 1. Infection : Infection at the site of the wound, lung and urinary infection. Infection risk is more if intestine is perforated before surgery, operated for colon and rectum, stent in placed in bile duct to relieve jaundice or intestinal joint is leaking. 2. Bleeding: The risk of bleeding during or after surgery is more if a patient taking blood-thinning medicine until the day of surgery or having liver dysfunction. Bleeding during surgery that may cause you to need blood transfusions. There is a risk of certain problems with transfusions, some of them serious. Still, some operations involve a certain amount of controlled blood loss. Bleeding can happen either inside the body (internally) or outside the body (externally). It can occur if a blood vessel sealed during surgery opens up or if a wound opens up. Serious bleeding may cause the person to need another operation to find the source of the bleeding and stop it. 3. Leakage from anastomosis (joint of anastomosis) & fluid collection in tummy. 4. Blockage of intestine (Intestinal obstruction) LIFE AFTER SURGERY Nutrition 1. Following treatment, you may feel the change in your taste. This improves over a time and we encourage having health food habits like fresh vegetables, fruits, and high protein diet. Exercise 1. Along with healthy food habits, we also encourage for exercise. Exercise improves your health in different ways: It improves your heart and circulation, makes your muscles stronger & makes you feel happier. You should do your regular activities like walking, and rather increase day by day. Weight lifting and strenuous exercise are avoided for initial 2-3 months. Follow up care 1. You'll need regular checkups after treatment for liver cancer. This help to find out any change in your recovery. Sometimes liver cancer comes back after treatment. Our healthcare team will check for return of cancer. Checkups may include a physical exam, blood tests, ultrasound / CT scan. 2. If you have any health problems between checkups, you should contact our healthcare team. Report to our health care team, if you have any redness/ swelling or discharge of any type of fluid from your operative incision site, pain abdomen, vomiting or fever, breathing difficulty etc.
If you have a question or concern after the test, please phone the Endoscopy Unit. Please consult your GP or go to your nearest A&E department if you develop severe abdominal pain, a fever or pass large amounts of blood after the test.

User visits the website and navigates to the "Appointment Booking" section.
After completing the form, the user submits their appointment request.
If the requested slot is available, the administrative staff confirms appointment.